Entradas
Mostrando las entradas de febrero, 2015
| Lista de correo. Espere su aprobación. |
| Consultar este grupo |
Laboratory Test Support for #Ebola Patients Within a High-Containment Facility
- Obtener vínculo
- X
- Correo electrónico
- Otras apps
Transmission of #Ebola Viruses
- Obtener vínculo
- X
- Correo electrónico
- Otras apps
#Ebola outbreak in Western Africa 2014: what is going on with Ebola virus?
- Obtener vínculo
- X
- Correo electrónico
- Otras apps
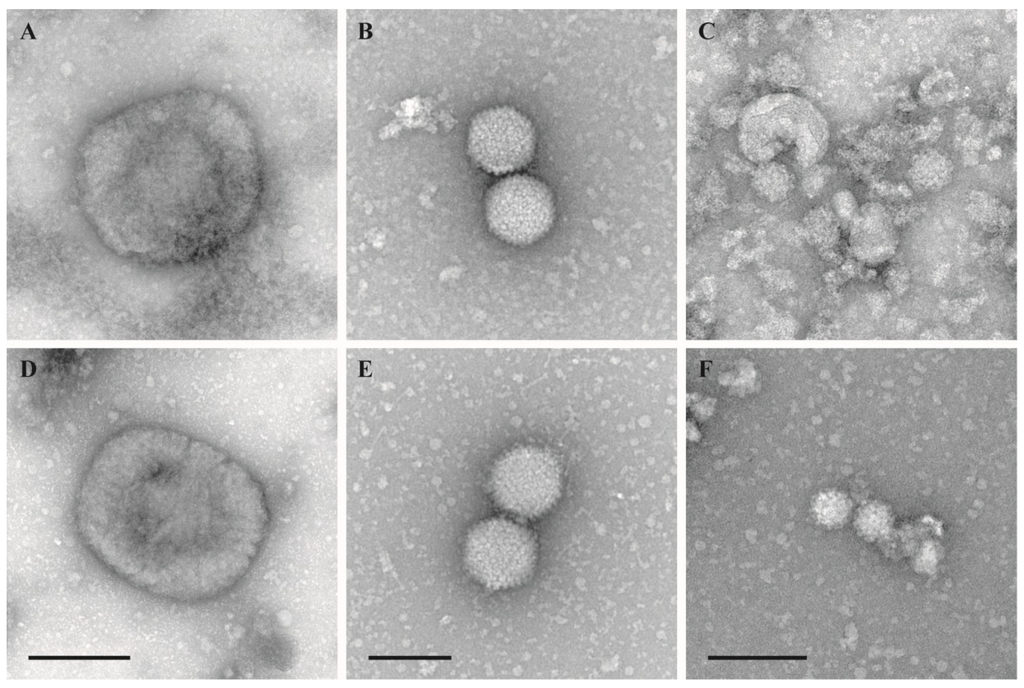
Evaluation of Virus Inactivation by Formaldehyde to Enhance Biosafety
- Obtener vínculo
- X
- Correo electrónico
- Otras apps
Guidance on regulations for the Transport of Infectious Substances 2015-2016
- Obtener vínculo
- X
- Correo electrónico
- Otras apps
Survey of Safety Practices Among Hospital Laboratories in Ethiopia
- Obtener vínculo
- X
- Correo electrónico
- Otras apps