Entradas
Mostrando las entradas de noviembre, 2018
Sesión académica AMEXBIO 2018
- Obtener vínculo
- Correo electrónico
- Otras apps
WHO Report on Surveillance of Antibiotic Consumption
- Obtener vínculo
- Correo electrónico
- Otras apps
Effective chemical virus inactivation compatible with accurate serodiagnosis of infections
- Obtener vínculo
- Correo electrónico
- Otras apps
Installing biosafety level 3 containment laboratories in low- and middle-income countries
- Obtener vínculo
- Correo electrónico
- Otras apps
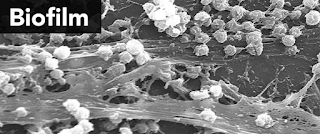
The effect of disinfectant formulation and organic soil on the efficacy of oxidising disinfectants against biofilms
- Obtener vínculo
- Correo electrónico
- Otras apps
Effect of Formaldehyde on Human Middle Ear Epithelial Cells.
- Obtener vínculo
- Correo electrónico
- Otras apps